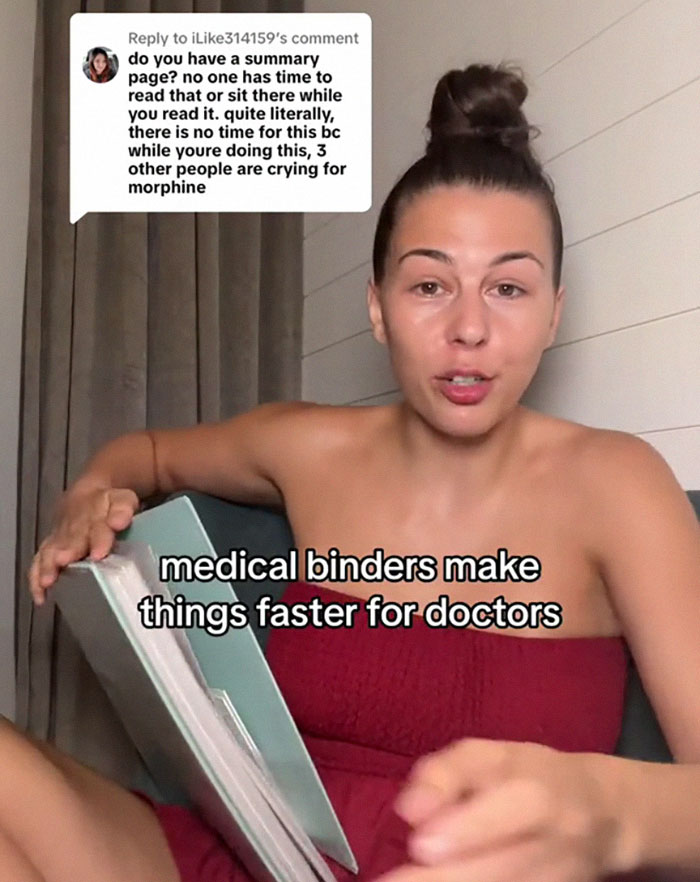
“Meet the Woman Who Took a Stand Against Inefficient Healthcare: Her Viral Medical Binder Sparks a National Conversation!”
Overall, an estimated 795,000 patients a year die or are permanently disabled due to misdiagnoses, according to a study published in BMJ Quality & Safety. However, some groups are more at risk than others.
Women and racial and ethnic minorities are 20% to 30% more likely than white men to experience a misdiagnosis, said Dr. David Newman-Toker, a professor of neurology at Johns Hopkins School of Medicine and the lead author of the BMJ study. “That’s significant and inexcusable,” he told KFF Health News.
Other research consistently confirms this bias.
For example, a study published in Academic Emergency Medicine found that women who visited the emergency room with severe stomach pain waited almost 33% longer than men with the same symptom.
Among minorities, Black people with depression are more likely than others to be misdiagnosed with schizophrenia. Additionally, minorities are less likely than white patients to be diagnosed early with dementia, depriving them of access to treatments that are most effective in the early stages of the disease.
“The vast majority of diagnoses can be made by getting to know the patient’s story really well, asking follow-up questions, examining the patient, and ordering basic tests,” said Hardeep Singh, a professor at Baylor College of Medicine and a researcher at Houston’s Michael E. DeBakey VA Medical Center. When speaking with people who’ve been misdiagnosed, “one of the things we hear over and over is, ‘The doctor didn’t listen to me.’”